Nearly every American carries measurable levels of so-called “forever chemicals” in their body. These compounds, known as PFAS (per- and polyfluoroalkyl substances), are synthetic chemicals engineered to resist heat, oil, stains, and water. That same resistance makes them exceptionally difficult for the human body to eliminate.
PFAS are found in nonstick cookware, fast-food wrappers, water-repellent clothing, carpeting, cosmetics, and even drinking water. Once they enter the body, many persist for years—circulating, accumulating, and quietly interfering with metabolism.
The organ that bears the greatest burden from these chemicals is the liver.
Fatty Liver Disease: Why PFAS and Modern Chemicals Target the Liver
The liver is your primary detoxification and metabolic control center. Every chemical absorbed through food, water, air, or skin eventually passes through liver tissue for processing.
PFAS disrupt liver health in several critical ways:
They interfere with the liver’s ability to package and export fat, causing fat to accumulate inside liver cells. When this process is disrupted, fat builds up in the liver, and if fat exceeds about 5% of the liver’s weight, it is considered steatosis or fatty liver disease.
They impair bile flow, slowing toxin elimination
They disrupt mitochondrial energy production, reducing the liver’s capacity to detoxify efficiently
They mimic or interfere with hormone signaling, worsening insulin resistance and metabolic dysfunction
Over time, this toxic interference contributes to fatty liver disease, inflammation, and impaired detoxification—often without obvious early symptoms.
Recently, what was once called nonalcoholic fatty liver disease (NAFLD) is now often referred to as steatotic liver disease, associated steatotic liver disease, or metabolic dysfunction-associated steatotic liver disease (MASLD).
These terms reflect the underlying metabolic causes and the strong association with metabolic syndrome, including obesity, type 2 diabetes, and high blood pressure. MASLD is defined as the buildup of extra fat in liver cells not caused by alcohol and is linked to these metabolic risk factors.
Dysfunction associated steatotic liver and metabolic dysfunction-associated steatotic liver disease are now recognized as umbrella terms for conditions where fat builds up in the liver due to metabolic dysfunction, and can progress to more severe forms like MASH (metabolic dysfunction-associated steatohepatitis) or cirrhosis. Experts do not fully understand why fat builds up in some livers and not others, nor why fat buildup in some livers turns into MASH.
Introduction to Liver Health
Your liver isn’t just another organ—it’s your body’s central detox hub, working around the clock to filter toxins, support digestion, and regulate metabolism. And here’s what most people don’t realize: maintaining liver health isn’t optional. It’s foundational to everything else your body does. Because when your liver gets overwhelmed, everything downstream suffers. We’re talking about the organ that processes every nutrient you consume and neutralizes every harmful substance that enters your system. Two of the most common ways this vital system breaks down? Nonalcoholic fatty liver disease (NAFLD) and alcoholic fatty liver disease. Both involve excess fat building up in liver tissue—and both can quietly progress from inflammation to scarring to complete liver failure if the underlying stress isn’t addressed.
This is where most people get it wrong. They think liver health is just about avoiding alcohol or eating “clean.” But in a world saturated with environmental toxins, processed foods, and constant metabolic stress, your liver needs strategic support, not just good intentions. A healthy diet and maintaining optimal weight aren’t just lifestyle suggestions—they’re your first line of defense against fatty liver and the cascade of complications that follow. These same strategies also help you sidestep metabolic syndrome—that dangerous cluster of conditions including elevated blood pressure, disrupted cholesterol, and insulin resistance—that dramatically increases your risk of liver cancer and other life-threatening complications. When you prioritize liver health, you’re not just supporting detoxification. You’re protecting yourself from the long-term consequences of liver failure and cancer. And that’s where real health resilience begins.
Nonalcoholic Fatty Liver Disease Is No Longer Just an Adult Problem
Fatty liver disease is now increasingly common in adolescents and young adults, especially in families with metabolic vulnerability. Research shows that certain PFAS compounds are strongly associated with increased fatty liver risk, liver inflammation, and early fibrosis.
This matters because the liver during adolescence and early adulthood is still adapting to:
Hormonal shifts
Growth and development signals
Increased metabolic demands
Chemical interference during this window places long-term stress on liver function that can persist into adulthood.
Microplastics: The Trojan Horse for PFAS Chemicals Exposure
PFAS rarely travel alone.
Microplastics—tiny fragments formed as plastics degrade—act as chemical delivery vehicles, carrying PFAS and other endocrine-disrupting compounds deep into the body.
Once inhaled or ingested, microplastics:
Bypass many natural detox barriers
Enter circulation through the lungs or gut
Deliver PFAS, BPA, phthalates, and flame retardants directly to the liver
Individuals with certain health conditions, such as obesity and metabolic syndrome, are at increased risk of developing MASLD when exposed to these chemicals.
The body has no natural mechanism to break down plastic polymers. That means detoxification depends on binding, bile flow, cellular repair, and elimination, not breakdown.
Symptoms and Diagnosis
Here’s what makes liver disease so dangerous: your liver can be failing, and you won’t even know it. This silent destruction happens because early-stage liver disease rarely announces itself. No dramatic symptoms. No obvious warning signs. Just quiet, progressive damage while you go about your daily life, thinking everything is fine. And that’s exactly why regular checkups aren’t just recommended—they’re critical. Nonalcoholic fatty liver disease and alcoholic fatty liver disease are master manipulators, progressing in complete silence. That fatigue you’ve been ignoring? The mild stomach discomfort you blame on stress? Those unexplained weight changes? Your liver might be trying to tell you something. But most people miss these whispers entirely.
Your doctor becomes a detective when liver disease is suspected. Blood tests reveal the truth—elevated liver enzymes that expose what’s really happening inside. But blood work is just the beginning. Imaging tests like ultrasound and MRI act as windows into your liver, detecting fat buildup and structural changes that shouldn’t be there. Sometimes, a liver biopsy becomes necessary—the ultimate investigation to assess exactly how much damage has occurred. This isn’t guesswork anymore. Risk factors like metabolic syndrome, high blood pressure, and high cholesterol get carefully evaluated during your physical exam and medical history review. Because here’s what most people don’t realize: early diagnosis and intervention aren’t just helpful—they’re your only real defense against further liver damage and the terrifying possibility of liver cancer. When your liver whispers, you need to listen. Before it stops talking altogether.
Why Detoxification Is About More Than Cleansing
True detoxification is not about forcing toxins out.
It’s about supporting the systems that safely move toxins through and out of the body.
That requires:
Functional bile flow
Healthy liver cells and mitochondria
Intact cell membranes
Adequate mineral balance
Binding and removal of toxins in the gut
This is where targeted supplementation becomes essential.
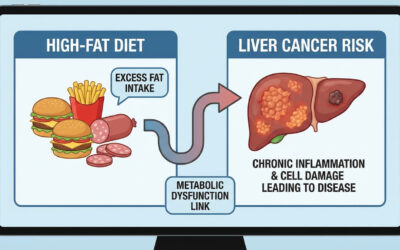
Health Risks and Liver Cancer
Liver cancer represents a serious biological threat for anyone carrying chronic liver disease—especially those whose livers show advanced scarring or cirrhosis. This isn’t some distant health concern. Conditions like Fatty Liver Disease, also known as metabolic dysfunction-associated steatohepatitis (MASH) and nonalcoholic steatohepatitis (NASH), are confirmed drivers of liver cancer risk. The key risk factors quietly accumulate: heavy alcohol use, elevated cholesterol, the presence of metabolic syndrome, and now forever chemicals—each one pushing your liver closer to cellular breakdown.
And that’s exactly why prevention becomes critical.
Adopting a strategically healthy diet, maintaining optimal weight, and avoiding modern day forever chemicals aren’t just lifestyle suggestions—they’re proven biological interventions that can dramatically lower your risk of liver cancer and other devastating complications. Organizations such as the American Liver Foundation and the National Institute of Diabetes and Digestive and Kidney Diseases provide essential intelligence on liver health, risk assessment, and targeted prevention strategies. By understanding and actively addressing these risks, you can take decisive action to protect your liver and safeguard your overall biological resilience.
Targeted Supplement Support for Chemical Detox & Fatty Liver
Because modern chemical exposure overwhelms multiple detox pathways at once, effective support must work at the level of liver function, cell membranes, bile flow, mineral balance, and toxin elimination—not just symptom relief. The following supplements are designed to support detoxification and fatty liver recovery by restoring the underlying cellular architecture that allows toxins and fat to move out of the body safely and efficiently.
Accelerated Liver Care®
Rebuilding Liver Function at the Cellular Level
The liver cannot clear toxins or export fat if its detox pathways are congested or inflamed. MASLD often has no symptoms, but when symptoms do occur, they may include fatigue and discomfort in the upper right side of the abdomen.
Accelerated Liver Care® is designed to support liver health supplements
Phase I and Phase II liver detoxification
Bile production and bile flow
Reduction of inflammatory signaling inside liver tissue
Cellular repair of hepatocytes (liver cells)
By improving bile flow and detox enzyme function, the liver becomes better able to:
Export fat instead of storing it
Process PFAS and hormone-disrupting chemicals
Reduce inflammation associated with fatty liver
MASLD can progress to a more advanced form called metabolic dysfunction-associated steatohepatitis (MASH), which causes the liver to swell and become damaged. MASH is characterized by inflammation, tissue damage, and the development of scar tissue in the liver—a process called fibrosis. If left untreated, fibrosis can progress to cirrhosis and further liver complications.
Supporting the liver is the foundation of any effective detox or fatty liver strategy.
Accelerated Cellular Detox® Powder
Binding and Removing What the Liver Releases
Detoxification does not end in the liver.
Once toxins are processed, they must be bound and removed in the gut—or they will be reabsorbed.
Accelerated Cellular Detox® Powder supports this critical step by:
Binding heavy metals, PFAS, and chemical byproducts
Reducing enterohepatic recirculation (toxin recycling)
Supporting gut-liver communication
This is especially important for fatty liver, because toxin recirculation:
Increases inflammatory load
Slows liver recovery
Worsens metabolic stress
Binding toxins allows the liver to keep detoxifying without becoming overwhelmed.
Acceleradine® Iodine
Restoring Metabolic Signaling and Chemical Resilience
Iodine deficiency is widespread—and deeply relevant to detox and fatty liver.
Iodine supports:
Thyroid hormone production and sensitivity
Estrogen and insulin receptor signaling
Displacement of toxic halogens (fluoride, bromine) that worsen the chemical burden
Without adequate iodine: To learn more, see Should Children Take Iodine Supplements.
Detox pathways slow
Metabolism becomes less efficient
Fat accumulates more easily in the liver
By restoring iodine sufficiency, the body becomes more resilient to chemical stress, supporting both metabolic health and detoxification capacity.
BodyBio® PC
Repairing Liver Cell Membranes and Exporting Fat
Phosphatidylcholine (PC) is essential for:
Liver cell membrane integrity
Bile formation
Fat transport out of the liver
Fatty liver is not just fat accumulation—it is impaired fat export.
BodyBio® PC supplies bioavailable phosphatidylcholine that:
Repairs damaged liver cell membranes
Supports bile production
Helps shuttle fat and toxins out of liver cells
Without adequate PC, fat becomes trapped inside hepatocytes, worsening fatty liver and slowing detox.
How Acceleradine® Iodine and BodyBio® PC Work Together at the Cell Membrane Level
Iodine and phosphatidylcholine are synergistic, not redundant.
Phosphatidylcholine provides the structural lipid framework of the cell membrane.
Iodine provides the functional signaling component within that lipid framework.
Together, they support the iodolipid value of the cell membrane, which refers to the membrane’s ability to:
Maintain proper hormone receptor signaling
Resist toxic halogen and chemical embedding
Regulate inflammation and oxidative stress
Support efficient fat metabolism and export
PC rebuilds and stabilizes the membrane itself.
Iodine integrates into that membrane environment, forming iodolipids that act as protective and regulatory molecules.
When both are sufficient:
Cell membranes become more resilient to PFAS, microplastics, and endocrine disruptors
Estrogen and insulin signaling normalize
Mitochondrial function improves
The liver can package, transport, and export fat instead of storing it
This combination is especially powerful for fatty liver because it addresses the problem at its root: damaged membranes, impaired signaling, and trapped lipids.
Why This Matters for Detox and Fatty Liver Recovery
Detoxification is not just about removing toxins—it’s about whether cells are structured well enough to let toxins and fat leave safely.
By pairing:
Acceleradine® Iodine (iodolipid signaling, halogen displacement, metabolic regulation)
withBodyBio® PC(membrane repair, bile support, lipid export)
you support detoxification at the cellular architecture level, where fatty liver and chemical accumulation actually begin.
This is why iodine and phosphatidylcholine together form a cornerstone of any serious strategy to address:
Fatty liver disease
PFAS and chemical overload
Hormone-driven metabolic dysfunction
Impaired detoxification
Accelerated Ancient Salt®
For those looking to improve their digestive wellness, check out our range of gut health supplements to support optimal digestive and gut health. Mineral Support for Detox and Fluid Balance
Detoxification is mineral-dependent.
In advanced liver disease, fluid buildup such as ascites and edema can occur due to impaired liver function, making proper mineral balance and hydration especially important.
Accelerated Ancient Salt® provides:
Trace minerals needed for enzyme activity
Support for adrenal and kidney function
Proper hydration and cellular electrical balance
Mineral depletion worsens detox fatigue, inflammation, and poor bile flow. Replenishing minerals helps the body process and eliminate toxins without crashing energy or stress systems.
Managing Stress and Liver Health
Managing stress isn’t just overlooked—it’s completely misunderstood when it comes to liver health. Chronic stress doesn’t simply worsen conditions like nonalcoholic fatty liver disease and alcoholic fatty liver disease. It systematically dismantles the liver’s ability to function by wreaking havoc on hormone balance and flooding the system with inflammatory compounds that the liver can’t clear fast enough. Most people think a healthy diet, regular exercise, and stress-reducing practices like meditation or yoga are enough to support liver function. But in a world saturated with environmental toxins and constant physiological stress, these surface-level approaches often miss what’s actually overwhelming the system.
Getting enough sleep and avoiding harmful substances like alcohol and tobacco barely scratches the surface of what’s required to actually protect your liver from the modern toxic load. Even the Environmental Protection Agency’s guidance on minimizing exposure to toxic chemicals like PFAS represents just a fraction of what’s quietly burdening liver pathways every single day. The truth is this: managing stress and making healthy lifestyle choices isn’t enough when your liver is already overwhelmed by the sheer volume of toxins, hormones, and inflammatory debris it’s trying to process. Real liver protection requires understanding that stress isn’t just emotional—it’s biochemical warfare against your body’s central detox hub. When you address the actual burden instead of just the symptoms, you don’t just lower your risk of liver disease and liver cancer. You restore your body’s natural intelligence to handle environmental and lifestyle challenges without breaking down.
Supporting Detox, Fatty Liver, and a Healthy Diet from All Angles
Reducing chemical exposure matters—but so does supporting the body’s ability to handle what it can’t avoid.
A comprehensive approach includes:
Liver pathway support
Toxin binding and elimination
Cell membrane repair
Thyroid and metabolic signaling
Mineral repletion
When these systems work together, the liver can:
Export fat more efficiently
Clear PFAS and environmental chemicals
Reduce inflammation
Restore metabolic balance over time
Final Thoughts
Forever chemicals didn’t become a problem overnight—and fatty liver doesn’t reverse overnight either.
But when detoxification is supported strategically and systemically, the body regains its ability to protect itself.
The goal isn’t aggressive cleansing.
It’s restoring the architecture that allows the liver to do its job—even in a chemically burdened world.
Sara Banta
Sara Banta is a Stanford University Graduate with a Degree in Economics and Psychology, and a certified Natural Supplement Expert & Graduate of the Institute for Integrative Nutrition. Sara is the Founder of Accelerated Health Products and host of the health & wellness podcast, Accelerated Health Radio.
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta
- Sara Banta